Borderline Personality Disorder (BPD) is characterized by a persistent pattern of instability in interpersonal relationships, self-image, and emotional regulation, together with marked impulsivity. It usually manifests in early adulthood, although many traits can already be observed during adolescence, and it appears across different contexts of a person’s life.
People with BPD show high sensitivity to environmental changes. The perception of separation, rejection, or loss of external support can trigger intense changes in how they see themselves, in their emotional state, thinking, and behavior. Strong efforts to avoid real or imagined abandonment are common.
Main clinical characteristics
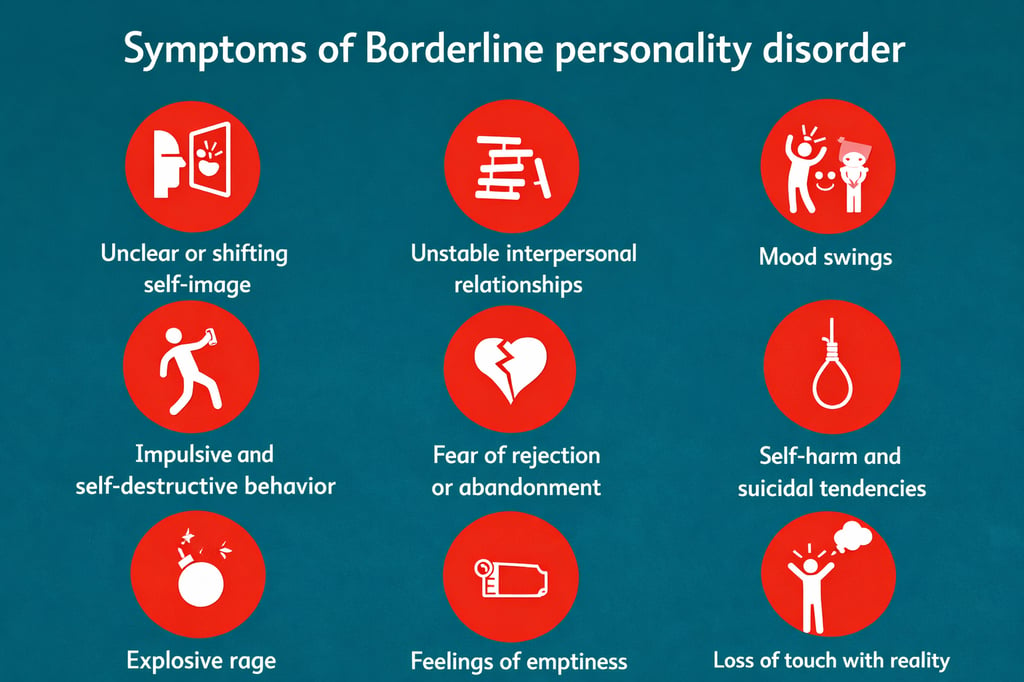
Among the most common features of BPD are:
Instability in self-image, life goals, and personal values
Intense and unstable interpersonal relationships
Predominantly dysphoric mood, with episodes of anger, distress, or despair
Chronic feelings of emptiness or boredom
Impulsivity across different areas of life
Prolonged periods of emotional well-being are usually infrequent
General therapeutic approach
Treatment of BPD requires an integrative and personalized approach, adapted to the characteristics and needs of each person. In many cases, it is beneficial to combine different therapeutic resources and, when possible, involve the family environment.
Intervention may include individual psychotherapy, psychoeducation, family work, and coordination with psychiatric services for pharmacological treatment when indicated. In more complex situations, the participation of a multidisciplinary team may be necessary.
To progress in the therapeutic process, the person’s motivation and the presence of a stable therapeutic relationship are especially important, as they help support the natural ups and downs of treatment.
Key aspects in the therapeutic process
Some fundamental elements commonly addressed during treatment include:
Establishing behavioral limits, which provide safety for the person and the therapeutic environment
Promoting autonomy, avoiding reinforcement of dependent behaviors
Developing resources to cope with new and emotionally intense situations
Although in many cases symptoms tend to decrease with age, treatment is essential to reduce personal and family suffering and to promote a more favorable course.
Psychoeducation and understanding of the disorder
Psychoeducation is a central pillar in the treatment of BPD. It allows the person to understand what is happening to them, identify patterns of functioning, and develop greater awareness of their emotions, thoughts, and behaviors.
The objective is to provide a clear and non-stigmatizing explanation of the disorder, facilitating self-observation, emotional regulation, and the maintenance of hope for change.
Final considerations
Borderline Personality Disorder does not define the person: it is something one has, not something one is. An accurate diagnosis and specialized treatment, based on understanding, psychoeducation, and continuous support, can lead to significant improvements in the quality of life of both the affected person and their environment


Borderline Personality Disorder
Intervention Approach at INTRA-TP




At INTRA-TP, personalized assessments are carried out, tailored to the situation and needs of each person. Clinical experience has shown that working with family members significantly facilitates recovery; therefore, whenever possible, the person’s environment is included in the therapeutic process.
In an initial phase, a family assessment is conducted in order to identify available resources, potential difficulties, and relevant behavioral patterns. Based on this evaluation, the work focuses primarily on psychoeducation, promoting a better understanding of the disorder and the associated relational dynamics.
However, this work with the family is not always possible. In some cases, family members or close individuals do not wish to become involved, considering that the problem should be addressed solely by the person affected. In these situations, intervention is carried out exclusively with the individual. In other cases, it is the person themselves who does not wish their environment to participate, a decision that is always respected. This does not prevent, when necessary, addressing specific questions or providing guidelines for managing certain situations.
The therapeutic approach may vary depending on the needs of the person seeking help or guidance, while always maintaining an integrative perspective.
At the individual level, the psychoeducational program for Borderline Personality Disorder developed by Dolores Mosquera, director of INTRA-TP, serves as the foundation. This program was published in 2004 under the title “Diamonds in the Rough II. Psychoeducational and Treatment Manual for Borderline Personality Disorder. A Structured Program for Professionals” (Pléyades Publishing). This program constitutes one of the pillars of the therapeutic work.
In addition, EMDR is used as a complementary approach, which has shown particularly promising results in this type of clinical presentation. Regarding pharmacological treatment, work is carried out in coordination with psychiatric services, both public and private, specialized in different areas.